HPV Infection
HPV Infection

Epidemiology
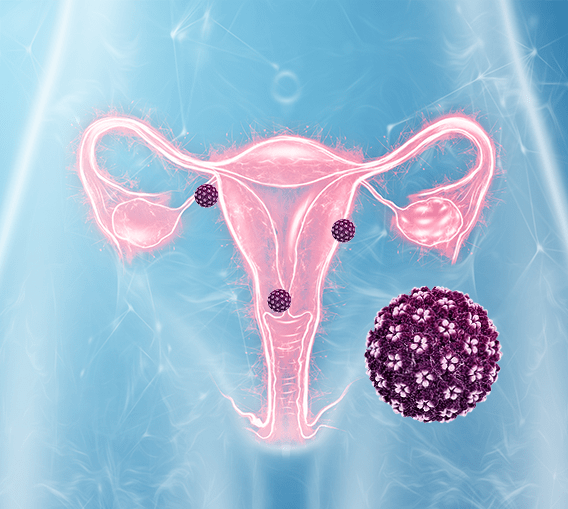
The human papillomavirus (HPV) is the world’s most common sexually transmitted infection: most sexually active people will be in contact with the virus at some point in their lives.
It is estimated that it can affect up to 30% of women under the age of thirty. A number that drops to 12% above this age.
Anyone who is sexually active can contract this infection, regardless of the number of partners and sexual practices they have had. Therefore, it is important to protect yourself properly by using a condom. However, once the virus is detected, it is impossible to determine when the infection occurred, since it can remain undetected by medical check-ups for years.
Although the prevalence of HPV in the male public is lower and studies confirming the data are lacking, it is estimated that 70% of men will be positive at some point in their lives.
Regardless of these numbers, in most cases there will be no serious consequences: 80% of them will spontaneously clear the virus within two years.
Classification
According to the World Health Organization (WHO), HPV strains can be classified into three broad categories, depending on how likely they are to cause cancer: low, medium or high-risk.
The different types of HPV are given numbers according to the order in which they were discovered. Of the 200-plus strains of HPV we know about, 40 infect the genital area, and 14 of them are high-risk. These high-risk strains have the potential to cause some type of lesions on the sexual organs that can progress into cancer.
LOW RISK HPV
These are the most common and those that can cause genital warts, known as condyloma acuminata, and mild changes in the female cervix. However, they do not have the potential to cause neither cancer nor serious lesions and, in most cases, the body will clear these low-risk strains on its own, within an average of two years. The most common of these are types 6 and 11.
MEDIUM RISK HPV
Medical sicence hasn’t yet been able to determine whether the risk from medium-risk HPV strains of causing some type of malignant change in the cells is high or low. Some strains of HPV in this category are 26, 53 and 73.
HIGH RISK HPV
These are the rarest, but most serious strains of HPV, since they have the potential to cause lesions on the cervix, which over time can develop into cervical cancer if they are not detected and treated properly on time.
High-risk strains are responsible for practically all cervical cancers; between 70% and 90% of those – the vagina and anus; 40% of those in the vulva and 20% of those in the oropharynx. HPV 16 and 18 are two most-common, being related to 70% of all cervical tumors.
What does the spontaneous HPV clearance rely on?
1. THE VIRAL TYPE:
There are many different types of HPV that are classified depending on their risk of developing into cervical cancer. Types 16 and 18 are the most common high-risk strains. Types are 6 and 11 are most common low-risk strains. Some types, like 16, are more difficult to clear than others. The viral type is the only factor which cannot be modified.
2. IMMUNE STATUS:
When our immune system, our natural defensive system is weakened, our body has a harder time fighting any external threat.
In most cases, our immune system will clear the virus within two years. However, sometimes our immune system doesn’t recognise the virus and it can remain undetected in the body for a long period of time. It is when HPV persists that it can give rise to lesions that, over time and without proper treatment, can progress to a more serious stage.
The reason for its difficult detection is that it is a small virus without a capsule, therefore, it does not have the envelope that would make it detectable by our natural immune system.
Its infective capabilities are determined by some predisposing factors that can allow the virus to copy its genetic material in our cells and, therefore, cause some type of injury.
The elimination of HPV by our immune system depends on four factors:
3. THE BALANCE OF THE VAGINAL MICROBIOTA:
It is recommended that a healthy vaginal microbiota is less diverse than the intestinal microbiota and should be mainly composed of Lactobacillus crispatus, a beneficial bacterium that is related to the remission of HPV. On the contrary, it’s been found that the of vaginal Gardanella has been related to greater persistence of the infection and greater likelihood of cervical lesions.
4. THE HISTOLOGICAL STRUCTURE OF THE UTERINE ECTOCERVIX:
HPV has more problems to infect the body if our cervix is well epithelialized and has non-existent transformation zones or limited extensions.
HPV prevention
There are four basic ways to prevent infection with HPV: the vaccine, regular gynaecological check-ups, the use of condoms and practising safe sexual life
1. THE VACCINE:
There are three existing vaccines to prevent HPV and it’s estimated that their widespread take up by adolescent girls who aren’t yet sexually active will drastically decrease the risk of contracting the infection and, thus, of developing cervical cancer (the most complete vaccine protects against the nine most common types of viruses, including seven high-risk and two low-risk). This is especially true for developing countries, whose mortality from cervical cancer is much higher than in Western countries.
Although the vaccine is most effective if given before the first sexual encounter, it can also be administered afterwards.
Vaccinating men is also recommended, since they are the major carriers of the virus.

2. GYNECOLOGICAL EXAMINATIONS
Having the recommended regular tests, known as cervical smear tests or pap tests, is very important, since these can detect the presence of HPV infection, even in its very early stages. This allows early treatment and is an important way to reduce the risk of lesions, or cancer, developing when the virus goes undetected for a long period of time.


3. THE USE OF CONDOMS
Using a condom reduces the chances of being infected with HPV, although everyone must be aware that its use does not fully prevent infection. It is important to bear in mind that, in 40% of cases, condoms are not used properly in the safest way, since they are often used only before the end of sexual intercourse to prevent ejaculating directly inside the vagina. It’s safer to put on a condom at the start of having sex and not taking it off until the end.

4. SEXUAL EDUCATION
This is an essential prevention tool for children and adolescents. The goal is to provide them with accurate information about the potential effects of HPV infection and how to practise safe sexual life.

In addition, maintaining healthy lifestyle habits that include a balanced diet and not smoking will help us reduce the chances of contracting HPV.
Transmission and myths about HPV
The main way for someone to become infected with HPV is through direct sexual contact, whether vaginal, anal or oral, or through the use of personal objects, such as sexual toys, that have been used by an infected person. and that haven’t been properly disinfected.

Although there are many false myths about this virus, the truth is that, based on the scientific evidence collected so far, it can be concluded that:
- Both women and men can contract and spread it
- The virus can go unnoticed and show no symptoms whatsoever
- The more sexual partners you have, the greater the risk of infection, even though it is possible to contract it with just a single sexual relationship.
- Although very rare, it is not impossible for a pregnant mother to transmit HPV to the baby at the time of delivery if she has warts in the birth canal, which could cause laryngeal papillomatosis to the newborn.

The virus has not been shown to be transmitted through:
- Swimming pools, hot tubs, gyms or any other type of sports environment.
- Toilet seats
- Kisses on the mouth
- Hugs or other non-sexual physical contact.
- Poor personal hygiene
- Toys, food or utensils

HPV Symptoms
How do you know if you’ve been infected with HPV??
As stated before, HPV often acts silently without the infected person knowing it’s there. Which is why it is so important to go to regular gynecological check-ups, which include a cytology.
If this test has a suspicious result, it will be necessary to carry out a medical follow-up, as well as any other tests that the specialist deems necessary.
It is important to bear in mind that infection by the different types of HPV is very varied and that its clinical manifestations can be different, including:
- Visible or clinical lesions.
- Non-visible or subclinical lesions, but diagnosed by some method, usually by examining the cells.
- Latent states, in which the infection is present, but in an inactive state.
What can happen if you have HPV?

Human papillomavirus infection follows an evolutionary course and is not synonymous with cancer, so a positive diagnosis should not be cause for alarm.
In addition, as we have mentioned so far, the prognosis and evolution of the infection will depend on many factors such as the strain of HPV that infects us, our immune system and our lifestyle.
Thus, when we are faced with an infection, very diverse lesions can appear, which can be symptomatic or asymptomatic depending on the HPV strain that infects us. Therefore, going to the gynaecologist or health specialist regularly is very important.
Condylomas or genital warts caused by low-risk strains of HPV
These are visible lesions that can appear on the cervix as well as on other areas of the female or male genitalia such as the vagina, vulva, urethra, anus, penis, perineum, larynx or skin.
They appear as irregular lesions, often described as cauliflower-shaped. They can be the same color as the skin, pink or white, single or multiple, soft, variable in size, or confluent.
Although genital warts must be treated and may cause discomfort to the patient, their prognosis is not very serious and they rarely lead to cancerous lesions
Cervical lesions caused by high-risk HPV
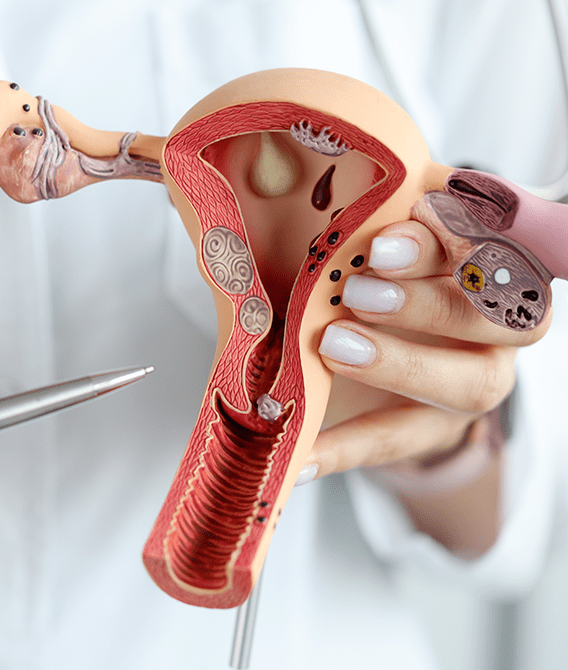
The cervix is the genital area which has a higher risk of persistent HPV infections.
Once the infection has occurred, the virus begins to divide within the cells of our cervix and change its morphology. The more cells that are altered, the greater the severity of the premalignant lesions that could lead to the appearance of cancer
According to the degree of progression, we can distinguish between:
- Low-grade lesions (LSIL) or less serious lesions, with a high probability of being spontaneously eliminated by our immune system
High-grade lesions (HSIL) or greater severity lesions, which are more likely to persist and possess a higher risk of progressing to cervical cancer.
In any case, the gynaecologist or expert in women’s health will be the one to determine the most appropriate course of action to follow, depending on the specific conditions of each patient.